Bone Marrow Stem Cells after Heart Attack Doesn’t Help
Introduction
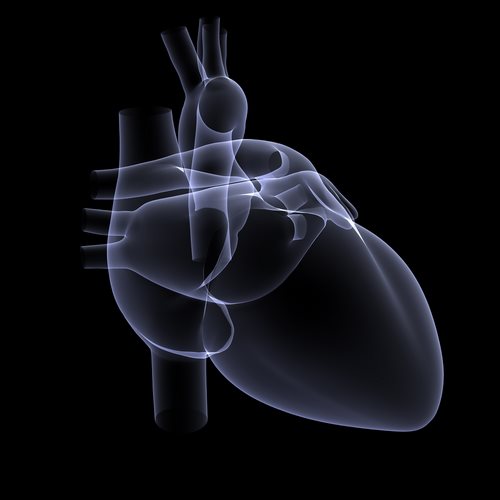
Bone marrow stem cells have been a source of much excitement in the medical community for their potential to help repair damaged heart tissue after a heart attack. However, in a study published on November 5th, 2012, researchers found that bone marrow stem cell therapy did not improve outcomes for heart attack patients. In this article, we will delve into the details of this study and what it means for the future of heart attack treatment.
The Study
The study, which was published in the Journal of the American Medical Association, involved 2,174 heart attack patients from 167 medical centers in 17 countries. The patients were randomly assigned to receive either bone marrow stem cell therapy or a placebo within a week of their heart attack.
The results of the study were surprising. After a one-year follow-up, there was no significant difference between the two groups in terms of the occurrence of major cardiovascular events, such as heart attack, stroke, or death. Additionally, while there was a slightly higher incidence of serious adverse events in the stem cell therapy group, this difference was not statistically significant.
What does this Mean for Heart Attack Treatment?
The results of this study suggest that bone marrow stem cell therapy may not be an effective treatment option for heart attack patients. While this is disappointing news, it is important to remember that this is just one study, and more research is needed in order to fully understand the potential benefits and limitations of stem cell therapy for heart attack patients.
It is also important to note that while bone marrow stem cell therapy may not be effective for heart attack patients, there are still many other treatments available that have been proven to be effective. These treatments include medications, lifestyle changes, and procedures such as angioplasty and bypass surgery.
Conclusion
Overall, the study published on November 5th, 2012, suggests that bone marrow stem cell therapy may not be an effective treatment option for heart attack patients. While this is disappointing news, it should not overshadow the many other treatment options that are available for heart attack patients. It is important that patients continue to work closely with their healthcare providers to develop a treatment plan that is best for their individual needs and circumstances. Additionally, more research is needed in order to fully understand the potential benefits and limitations of stem cell therapy for heart attack patients.
On November 5, 2012, the National Institutes of Health announced that patients who receive stem cells from their own bone marrow three to seven days after a heart attack do not show greater heart function within six months.
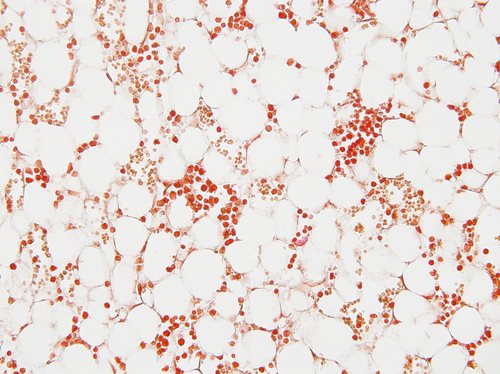
The medical trial that looked into the treatment was called the Transplantation in Myocardial Infarction Evaluation (TIME). The trial had similar results to a previous study performed by TIME. The study looked into the effects of autologous stem cells, which are produced in bone marrow.
Sonia Karlatos, Ph.D., the deputy director of NHLBI’s Division of Cardiovascular Sciences, stated: “Heart stem cell therapy research is still in its infancy, and results from early trials have varied greatly due to differences in the numbers of stem cells injected, the delivery methods used, and the compositions of the study populations.” With the results from both of the TIME studies, Karlatos mentioned, “This standard will inform the next steps in research on the use of stem cells to repair damaged hearts.”
Researchers with TIME enrolled 120 volunteers between July 2008 and February 2011. The average age of the participants was 57, and 87.5 percent of the participants were male. All of the volunteers had moderate or severe blockage of the left ventricles and has received stents after heart attacks. The volunteers were assigned to four groups:
• group 1: injection of stem cells three days after heart attack
• group 2: injection of placebo three days after heart attack
• group 3: injection of stem cells seven days after heart attack
• group 4: injection of placebo seven days after heart attack
The participants that received stem cells were injected with 150 million stem cells 8 hours after the cells were taken from the marrow.
Even though the results were unsuccessful, CCTRN member Jay Travese, M.D., stated: “With this baseline now set, we can start to adjust some of the components of the protocol to grow and administer stem cells to find cases where the procedure may improve function.”
Source: National Institutes of Health